Team Members Guide
Dubuque Non Union Team Members | Health, dental, and vision insurance, life and disability insurance, and programs to help save for the future, such as 401(k) and Health Savings Account (HSA)
2024 Benefit Guide DUBUQUE NON-UNION TEAM MEMBERS Copyright ® 2024 UnityPoint Health. All Rights Reserved. ® SM trademarks of UnityPoint Health. 003465j4-1 05/24 CS
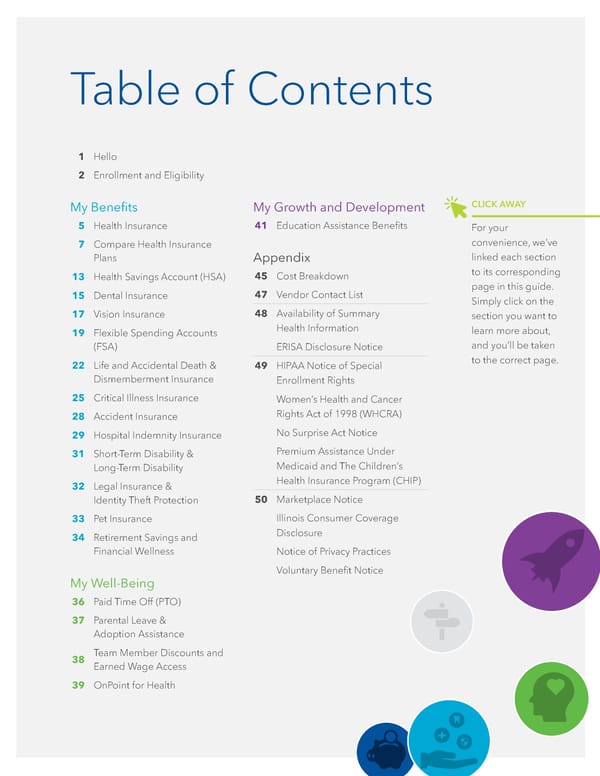
Table of Contents 1 Hello 2 Enrollment and Eligibility My Benefits 5 Health Insurance 7 Compare Health Insurance Plans 13 Health Savings Account (HSA) 15 Dental Insurance 17 Vision Insurance 19 Flexible Spending Accounts (FSA) 22 Life and Accidental Death & Dismemberment Insurance 25 Critical Illness Insurance 28 Accident Insurance 29 Hospital Indemnity Insurance 31 Short-Term Disability & Long-Term Disability 32 Legal Insurance & Identity Theft Protection 33 Pet Insurance 34 Retirement Savings and Financial Wellness My Well-Being 36 Paid Time Off (PTO) 37 Parental Leave & Adoption Assistance 38 Team Member Discounts and Earned Wage Access 39 OnPoint for Health CLICK AWAY For your convenience, we’ve linked each section to its corresponding page in this guide. Simply click on the section you want to learn more about, and you’ll be taken to the correct page. My Growth and Development 41 Education Assistance Benefits Appendix 45 Cost Breakdown 47 Vendor Contact List 48 Availability of Summary Health Information ERISA Disclosure Notice 49 HIPAA Notice of Special Enrollment Rights Women’s Health and Cancer Rights Act of 1998 (WHCRA) No Surprise Act Notice Premium Assistance Under Medicaid and The Children’s Health Insurance Program (CHIP) 50 Marketplace Notice Illinois Consumer Coverage Disclosure Notice of Privacy Practices Voluntary Benefit Notice
| 1 | hello. UnityPoint Health is proud to offer you a comprehensive TOTAL REWARDS PROGRAM. Total Rewards is the value provided to our team members and their families throughout their career at UnityPoint Health by combining Compensation, Benefits, Personal Growth and Development, Recognition, Well-Being, and Purpose into one, simple program. UnityPoint Health is committed to providing benefits that support our team members from various backgrounds, experiences, and identities. We offer benefits aimed to meet the needs of all of our team members and their families. How to Use this Guide We know there is a lot of information in this guide, and you may be feeling a little overwhelmed. We put together a few tips for how to get the most out of this guide as you prepare to select your benefits. › Use the Table of Contents Click on the title of the benefit you want to learn more about for quick navigation around the guide. › Know Where to Get the Most Up to Date Information Please remember that these enrollment guides are sometimes updated throughout the year. For the most up to date information, head to unitypoint.org/totalrewards. › AskHR is Here to Help! If you have questions about anything in the enrollment guide, reach out to AskHR by creating a case in Lawson or by calling (888) 543-2275.
| 2 | * When enrolling a domestic partner, you will be required to verify and acknowledge that they are eligible for the plans you have selected. After you complete your enrollment our HR Shared Services team will reach out within a few business days to advise on the next steps towards verifying your domestic partner. **Applies if not covered by other government programs and meets the eligibility requirements as defined by each benefit plan. Enrollment and Eligibility Eligible team members have 30 days from their start date to enroll in benefits using the Lawson portal. Benefits coverage begins the first day of the month following your start date. You can find a link to Lawson and instructions for how to enroll on the Total Rewards Site. Who is Eligible You are eligible to enroll in UnityPoint Health benefits if you are in a benefits- eligible status. You are eligible for benefit coverage if you are: FULL-TIME team member who is regularly scheduled to work 64 hours or more per pay period. (0.8 - 1.0 FTE) PART-TIME team member who is regularly scheduled to work 32-63 hours or more per pay period. (0.4 - 0.79 FTE) Dependents In most cases, you can also cover your eligible dependents. If adding a spouse/ domestic partner or dependent child, UnityPoint Health highly encourages adding their social security number (identification number) into their dependent profile. Dependent Verification You may be asked to verify your dependent’s eligibility by providing documentation. If asked to do so, you must submit all documents within 30 days of request or risk having your dependents removed from the elected benefit. Eligible dependents include: › Spouse/partner (spouse, civil union partner, domestic partner*, common law spouse) › Your children under age 26. › Unmarried children of any age who are unable to support themselves because of a physical or mental disability.** Working Spouse Surcharge Team members that choose to enroll a working spouse or domestic partner who is eligible for health insurance coverage through their employer will pay a $75 working spouse surcharge. The $75 surcharge only applies to medical coverage and will be added to your per pay period medical premium.
| 3 | Domestic Partner Imputed Income If you choose to add your domestic partner to your medical and/or dental coverage, you will be responsible for imputed income tax on the difference in the employer premium for the additional coverage. Status and Benefit Changes You can change your coverage during the year if you have a qualifying life event. The changes you may make depend on the type of qualifying event that occurs. If you experience a qualifying life event and wish to make changes to your benefits, you must declare a life event through Lawson within 30 days from the date of the event (60 days for the birth of a child, adoption, or adoption placement). Team members are allowed to make changes mid- year between plan options under health insurance or dental insurance. For example you may change from the Network Plan to the Health Savings Plan (HSA) or vice versa. Note: Deductible and maximum out of pocket accumulators will not transfer between plan options, team members will be responsible for any excess health saving account contributions and team members are not able to change flexible spending account annual election amounts. Qualifying Life Events › Marriage, divorce, or legal separation › Birth or addition of an eligible child › Loss of other coverage › New eligibility for other coverage › Qualified medical child support order › Status changes › Commencement or return from an unpaid leave of absence STATUS CHANGES Current team members who are newly benefit eligible have 30 days from their status change date to enroll in benefits. If moving from a full-time to part-time position or vice versa you have 30 days from status change date to request a change to your health insurance through AskHR. Transferring Employment Within UPH Affiliates If you transfer employment to another UnityPoint Health affiliate, your benefits will continue unchanged if you continue to meet eligibility requirements. You cannot make changes to your benefit elections if you transfer employment as this is not a qualifying event for making changes during the year. Dependent Eligibility Eligibility for your dependent begins or ends with: › Change in residence or place of work resulting in change in health insurance availability › Death of spouse/domestic partner or child LIFE EVENT GUIDE For additional information check out the Qualified Life Event Guide
My Benefits Health, dental, and vision insurance, life and disability insurance, and programs to help save for the future, such as 401(k) and Health Savings Account (HSA)
| 5 | Health Insurance Key Health Care Terms We’ve compiled this list of health care terms to help you navigate this section of the enrollment guide: › Deductible: Dollar amount you must pay for covered care each calendar year before the medical plan pays benefits for services. The deductible doesn’t apply to every service so be sure to check out the summary schedule of benefits. Under the Network plan, the family must collectively satisfy the family deductible. Additionally, each family member has an individual deductible in addition to the overall family deductible. Meaning if an individual in the family reaches his or her deductible before the family deductible is reached, his or her services will be paid by the insurance company. Under the Health Savings plan (HSA), the family deductible must be reached, either by an individual or by the family, before services will be paid by the insurance company. There is no individual deductible under the HSA plan. › Coinsurance: Percentage of the cost for eligible medical expenses that you pay after you meet the deductible. For example, under the Health Savings Plan, after you meet the deductible, the plan will pay 80% of covered costs and you pay the remaining 20% up to the plan’s out-of-pocket maximum limit. The 20% is your coinsurance. › Copayment (or copay): A fixed amount that you must pay for a service. Copays can vary depending on the service you receive. › Network Providers: Providers who have agreed to lower rates for services. The UnityPoint Health medical plans provide benefits for covered services provided by network providers. › Out-of-Pocket Maximum (OOPM): Maximum dollar amount that you pay for eligible expenses in a calendar year. The plan pays 100% of eligible expenses for the rest of the calendar year after the out-of-pocket maximum is reached - providing financial protection for you by limiting your out-of-pocket expenses in a given calendar year. The out-of-pocket limit is a combined amount for both medical and prescription coverage under each medical plan. Which Medical Plan is the Best Choice for Me? You will have the choice to waive medical coverage or select coverage from one of two HealthPartners medical plans. Both medical plans: › Cover the same basic medical services › Cover the same network of doctors, hospitals and health care specialists who deliver quality care according to network standards and have agreed to lower, preferred rates for covered services. However, depending on the plan selected, your share of the cost of the medical services you receive differs. NETWORK PLAN › Higher biweekly premium cost for coverage › Cost of care (deductible amounts and out-of pocket limit) lower than the Health Savings Plan HEALTH SAVINGS PLAN (HSA) › Pay less in biweekly premium cost for coverage › Cost of care (deductible amounts and out-of-pocket limit) will be higher than the Network Plan › UnityPoint Health contributes to your Health Savings Account to help offset out-of- pocket costs
| 6 | Health Insurance, continued Preventive Care Benefits Working in health care, we know how adopting a healthy lifestyle can help us stay well and live better. Therefore, it is important that you periodically receive physical exams and health screenings that help you identify health risks early to avoid developing more serious problems down the road. The following preventive services are covered at 100%, with no deductible, whether you enroll in the Health Savings Plan or the Network Plan as long as you see a network provider: › Routine health exams and periodic health assessments › Well-child visits › Routine screening procedures for cancer › Routine hearing exams › Adult immunizations › Obesity screenings and management › Women’s preventive health services including all FDA approved contraceptive methods as prescribed by a physician Walk-In & Virtual Care Our insurance plans cover walk-in and virtual care if you are unable to see your primary care provider or it is outside of clinics operating hours. Walk- In Care: Our Urgent Care, Express or Express Care locations treat minor medical problems and injuries that are not life-threatening. You can save time by reserving your spot online. Click here to search for a walk-in care clinic near you. Virtual Care in MyUnityPoint: See a provider through video with Virtual Urgent Care for minor medical problems that are not life-threatening. Please note: some conditions and certain age groups can’t be treated through virtual care. Team members must be in Iowa to use this service. For more information visit unitypoint.org/virtualcare.

| 7 | * Funds can be carried over year-to-year if you don’t use them for medical or pharmacy expenses like meeting deductibles and out-of-pocket limits for the team member, spouse, or tax dependent. The spouse and tax dependent don’t have to be covered under a UnityPoint Health Medical Plan to be able to use HSA funds. Refer to the Health Savings Account section to learn more. ** UnityPoint Health advances the employer contribution to your account when you enroll in the Health Savings Plan which allows you to have access to those funds immediately. This amount is prorated based on your benefit eligibility date and number of months remaining in the year. *** Premium amounts shown above do not include the working spouse surcharge. For more information, please refer to the Enrollment and Eligibility section. Health Insurance, continued Compare Health Insurance Plans Deductibles, Out-of-Pocket Maximums and Premiums HEALTH SAVINGS PLAN (HSA) NETWORK PLAN Annual Medical Deductible Individual Limit $2,000 $900 Family Limit $3,500 $1,800 Annual Out-of-Pocket Limit (includes medical deductible) Individual Limit $4,250 $3,125 Family Limit $7,000 $6,750 Health Savings Account (HSA)* Eligibility Eligible Not Eligible UnityPoint Health Contribution** $750 for EE Only Coverage; $1,500 for EE+ C, EE+S/DP, or Family Coverage Your Personal Contribution (Not required) Up to $3,400 for EE Only; Up to $6,800 for EE+C, EE+S/DP, or Family Additional catch-up contribution of $1,000 (if age 55 or older) Cost of Coverage / Per Pay Period Full-Time Premium Amounts*** (0.80 - 1.0 FTE) Part-Time Premium Amounts*** (0.4 - 0.79 FTE) Full-Time Premium Amounts*** (0.80 - 1.0 FTE) Part-Time Premium Amounts*** (0.4 - 0.79 FTE) Employee Only $47.05 $71.63 $79.82 $119.73 Employee + Child(ren) $92.55 $138.81 $154.71 $232.07 Employee + Spouse/DP $112.50 $168.75 $188.09 $282.13 Family $154.27 $231.41 $257.94 $386.91
| 8 | Health Insurance, continued Compare Health Insurance Plans, continued The percentages in the following table are the percentages you pay. For example, if you see “20%” that means the plan pays 80% and the remaining 20% is your responsibility. If you see “100% covered” that means there is no member responsibility for that type of care or service. Anytime you see “after deductible is met,” that means the annual medical deductible for the plan must be met before the plan will pay. Please keep in mind that these do not reflect any services not covered by the plan or benefit reductions caused by not complying with preauthorization. HEALTH SAVINGS PLAN (HSA) NETWORK PLAN Network Facilities and Providers Network Facilities and Providers Wellness and Preventive Care 100% Covered 100% Covered Annual Medical Deductible Individual Limit $2,000 $900 Family Limit $3,500 $1,800 Annual Out-of-Pocket Limit (includes medical deductible) Individual Limit $4,250 $3,125 Family Limit $7,000 $6,750 Office Visits Primary Care Provider (PCP) 20% after deductible is met $10 or $50 copay (See zip code table to determine if higher copay applies) Specialist 20% after deductible is met $50 copay Chiropractic Care (Up to 5 visits per year) 20% after deductible is met $10 copay Infertility Services 20% after deductible is met, up to a $15,000 lifetime maximum 20% after deductible is met, up to a $15,000 lifetime maximum Urgent Care 20% after deductible is met $20 copay* Emergency Room Services 20% after deductible is met 1-3 visits: $150 copay, then 20% after deductible is met 4-5 visits: $400 copay, then 30% after deductible is met 6 or more visits: $600 copay, then 40% after deductible is met * Primary Care Provider (PCP) copay may apply at some locations if not able to bill as urgent care.
| 9 | Health Insurance, continued Compare Health Insurance Plans, continued HEALTH SAVINGS PLAN (HSA) NETWORK PLAN Ambulance 20% after deductible is met $0 copay Virtual Care Services Virtual Care Office Visits 20% after deductible is met $10 or $50 copay See zip code table to determine if higher copay applies Virtual Care Urgent Care 20% after deductible is met $10 copay Mental Health and Substance Abuse Outpatient Office Visits 20% after deductible is met $10 copay Inpatient 20% after deductible is met 20% after deductible is met Outpatient Therapy Services PT/OT 20% after deductible is met $10 copay Cardiac Rehab/Dialysis 20% after deductible is met 20% after deductible is met Outpatient Imaging and Lab Diagnostic Testing (CT/PET Scan/MRI) 20% after deductible is met 20% after deductible is met Diagnostic X-Rays 20% after deductible is met 20% after deductible is met Labs: Preventive 100% coverage 100% coverage Labs: Diagnostic 20% after deductible is met 100% coverage Hospice 20% after deductible is met 20% after deductible is met Durable Medical Equipment (DME) 20% after deductible is met 20% after deductible is met
| 10 | Health Insurance, continued Compare Health Insurance Plans, continued HEALTH SAVINGS PLAN (HSA) NETWORK PLAN Prescription Drug Coverage Retail Clinic (Up to 30-day supply) Any Retail Pharmacy (excluding CVS pharmacies) Tier 1 Pharmacies Tier 2 Pharmacies (excluding CVS pharmacies) Formulary Generic 20% after deductible is met $10 copay $20 copay Formulary Brand 20% after deductible is met $40 copay $50 copay Specialty Drugs Designated Network Specialty Pharmacy only Designated Network Specialty Pharmacy only Formulary Specialty 20% after deductible is met $60 copay Up to 90-Day Supply HealthPartners Mail Order Pharmacy and UPH Affiliate HealthPartners Mail Order Pharmacy UPH Affiliate Pharmacies Formulary Generic 20% after deductible is met $30 copay $25 copay Formulary Brand 20% after deductible is met $120 copay $100 copay
| 11 | Health Insurance, continued About Your Medical Plan’s Prescription Drug Coverage If you take any medications regularly, prescription drug costs can add up to a significant part of your overall health care expenses. Knowing how your medical plan’s prescription drug coverage works and what to do to manage costs can help you make smarter purchases and lower your out-of-pocket costs. Here are a few items that are important to note: › Under the Network Plan, lower Tier 1 copays for generic or brand drug fills ($10 copay for formulary generic drugs and $40 copay for formulary brand drugs) will apply when having prescriptions filled at a UnityPoint Health or Hy-Vee pharmacy. In addition, Tier 1 copays will apply to any retail pharmacy located outside a 15 mile radius of a UnityPoint Health or Hy-Vee pharmacy. › Please note, to further support our rural communities and those with limited access to a UnityPoint Health or Hy-Vee pharmacy, the lower Tier 1 copays explained above will apply to a few additional pharmacies. For a full list, please click here. › Under the Network Plan, higher Tier 2 copays for generic or brand drug fills ($20 copay for formulary generic drugs and $50 copay for formulary brand drugs) will apply when having prescriptions filled at any retail pharmacy located within a 15 mile radius of a UnityPoint Health or Hy-Vee pharmacy. › Both medical plans only provide coverage for formulary drugs. The formulary is compiled by a group of doctors and pharmacists. Medications are reviewed and approved for the formulary based on medical effectiveness and cost, which helps keep costs affordable for you. If you’d like to check to see if your prescriptions are on the formulary list, head to healthpartnersunitypointhealth.com/uph and click “Check Prescriptions.” › Coverage at CVS pharmacies (including Target locations) is not provided. › The Rx shopping tool is an online prescription cost- saving tool. It helps you find the lowest cost for medicines, based on your current health plan. Visit healthpartnersunitypointhealth.com/uph and log on to your myHealthPartners account. Once logged on, you’ll be able to use the Rx shopping tool. › A UnityPoint Health Medication Therapy Management (MTM) pharmacist can help you focus on your medicines to make sure they are a good fit for you and your health conditions. Your personal pharmacist will work with you and your care team to check that your medicines, doses, and schedules meet your needs. Your pharmacist will also make sure that your drugs work well together and aren’t causing side effects. Visits can often be provided by phone or video conference, making them easier to fit into your schedule. Working with a pharmacist on a regular basis might also save you money on your medicine copays.
| 12 | Health Insurance, continued Zip Code Table for PCP Office Visit Copay and Provider Network If you enroll in the Network Plan and your home residence zip code is bolded in the table below, your Primary Care Provider (PCP) office visit copay will increase to $50 if you choose to see an in-network, non-UnityPoint Health PCP. If your PCP Office Visit is to a UnityPoint Health PCP, your copay will remain $10. › If your home residence zip code is NOT bolded in the table below, your Primary Care Provider (PCP) office visit copay will be $10 as long as you see an in-network PCP. Your home residence zip code will also determine your provider network access. To locate in network providers visit healthpartnersunitypointhealth.com/uph and log on to your myHelathPartners account. Once logged on, select find a doctor and pick the appropriate plan. If your home residence zip code is listed below, you will pick the “In Zip Code Table” plan. Team members who reside within the zip code table and have dependents residing in a different zip code should contact AskHR to start the process of authorizing providers in that area. QUICK SEARCH For a quick way to see if your home residence zip code is listed in the table below, use “ctrl+F” on your keyboard, which will open a search bar. Once that appears, enter your home residence zip code and press “enter”. 50001 50002 50003 50005 50006 50007 50009 50010 50011 50012 50013 50014 50021 50023 50026 50027 50028 50029 50031 50032 50033 50034 50035 50036 50037 50038 50039 50040 50041 50043 50044 50046 50047 50048 50049 50050 50051 50054 50055 50056 50057 50058 50060 50061 50062 50063 50064 50066 50068 50069 50070 50071 50072 50073 50075 50078 50099 50101 50102 50104 50105 50106 50107 50109 50111 50112 50115 50116 50118 50119 50120 50122 50124 50125 50126 50127 50128 50129 50130 50131 50132 50134 50135 50136 50137 50138 50139 50141 50142 50143 50145 50146 50148 50149 50150 50151 50152 50153 50154 50156 50157 50158 50160 50161 50162 50163 50164 50166 50167 50168 50169 50170 50171 50173 50174 50201 50206 50207 50208 50210 50211 50212 50213 50214 50216 50217 50219 50220 50223 50225 50226 50227 50228 50229 50230 50231 50232 50233 50234 50235 50236 50237 50238 50239 50240 50241 50242 50243 50244 50246 50247 50248 50249 50250 50251 50252 50254 50256 50257 50258 50259 50261 50263 50264 50265 50266 50268 50269 50271 50275 50276 50277 50278 50301 50302 50303 50304 50305 50306 50307 50308 50309 50310 50311 50312 50313 50314 50315 50316 50317 50318 50319 50320 50321 50322 50323 50324 50325 50327 50328 50329 50330 50331 50332 50333 50334 50335 50336 50339 50340 50359 50360 50361 50362 50363 50364 50367 50368 50369 50380 50381 50391 50392 50393 50394 50395 50396 50398 50441 50501 50510 50516 50518 50519 50520 50521 50523 50524 50525 50526 50527 50529 50530 50532 50533 50535 50538 50540 50541 50542 50543 50544 50545 50546 50548 50551 50552 50554 50557 50558 50560 50561 50562 50563 50566 50567 50568 50569 50570 50571 50573 50574 50575 50576 50577 50579 50581 50582 50583 50585 50586 50588 50591 50592 50593 50594 50595 50599 50601 50602 50604 50607 50608 50609 50611 50612 50613 50614 50616 50619 50621 50622 50623 50624 50626 50627 50629 50630 50631 50632 50633 50634 50635 50636 50638 50641 50642 50643 50644 50647 50648 50649 50650 50651 50654 50655 50657 50658 50660 50661 50662 50664 50665 50666 50667 50668 50669 50670 50671 50672 50673 50674 50675 50676 50677 50680 50681 50682 50701 50702 50703 50704 50706 50707 50801 50830 50831 50845 50849 50858 50859 50861 50936 50940 50947 50950 50980 50981 50982 50983 51001 51002 51003 51004 51005 51006 51007 51008 51009 51010 51012 51014 51016 51018 51019 51020 51022 51024 51025 51026 51027 51028 51029 51030 51031 51033 51034 51035 51036 51037 51038 51039 51041 51044 51046 51047 51048 51049 51050 51051 51052 51053 51054 51055 51056 51058 51060 51061 51062 51063 51101 51102 51103 51104 51105 51106 51108 51109 51111 51234 51238 51239 51245 51250 51401 51431 51433 51436 51439 51440 51443 51444 51445 51448 51449 51450 51451 51452 51453 51455 51458 51459 51460 51461 51462 51463 51466 51483 51572 51609 52001 52002 52003 52004 52030 52031 52032 52033 52035 52036 52037 52038 52039 52040 52041 52042 52043 52044 52045 52046 52048 52049 52050 52052 52053 52054 52056 52057 52060 52064 52065 52066 52068 52069 52073 52074 52076 52078 52079 52142 52147 52164 52171 52202 52203 52204 52205 52206 52207 52208 52209 52210 52211 52212 52213 52214 52215 52216 52217 52218 52219 52220 52221 52222 52223 52224 52225 52227 52228 52229 52232 52233 52236 52237 52243 52244 52249 52251 52252 52253 52254 52255 52257 52301 52302 52305 52306 52307 52309 52310 52312 52313 52314 52315 52316 52317 52318 52320 52321 52322 52323 52324 52325 52326 52328 52329 52330 52332 52333 52334 52335 52336 52337 52338 52339 52340 52341 52342 52344 52345 52346 52347 52348 52349 52351 52352 52354 52355 52356 52358 52361 52362 52401 52402 52403 52404 52405 52406 52407 52408 52409 52410 52411 52497 52498 52499 52501 52530 52531 52536 52537 52553 52561 52569 52701 52720 52721 52722 52726 52727 52728 52729 52731 52733 52734 52736 52739 52742 52745 52746 52747 52748 52749 52750 52751 52752 52753 52754 52755 52756 52757 52758 52759 52760 52761 52765 52766 52768 52769 52772 52773 52774 52776 52777 52778 52801 52802 52803 52804 52805 52806 52807 52808 52809 53554 53803 53804 53806 53807 53808 53810 53811 53812 53813 53816 53818 53820 61025 61036 61075 61201 61232 61233 61234 61235 61236 61238 61239 61240 61241 61242 61244 61250 61254 61256 61257 61258 61259 61262 61263 61264 61265 61266 61272 61273 61274 61275 61276 61277 61278 61279 61281 61282 61283 61284 61314 61336 61344 61345 61361 61369 61375 61413 61414 61419 61421 61424 61427 61432 61434 61443 61449 61451 61465 61468 61479 61483 61486 61489 61491 61516 61517 61519 61520 61523 61524 61525 61526 61528 61529 61530 61531 61533 61534 61535 61536 61537 61539 61540 61541 61542 61543 61544 61545 61546 61547 61548 61550 61552 61553 61554 61555 61559 61560 61561 61564 61565 61568 61569 61570 61571 61572 61601 61602 61603 61604 61605 61606 61607 61610 61611 61612 61614 61615 61616 61625 61654 61725 61729 61732 61733 61734 61742 61747 61755 61759 61771 62682 Note: The Family Medicine clinic in Grinnell, IA is eligible for a $10 copay.
| 13 | Health Savings Account (HSA) What are the benefits of establishing a Health Savings Account (HSA)? There are many benefits of establishing an HSA. Some of the top benefits include: › Contributions reduce taxable income, funds grow tax-free and distributions for qualified expenses are not taxed. › UnityPoint Health makes a contribution to your health savings account. › The balance can roll over from year to year. Unlike a flexible spending account (FSA), the HSA is not a “use it or lose it” account. › You can change or update contributions throughout the year. › HSA funds belong to you even if you leave UnityPoint Health, change medical plans, or retire. Receive and Make Contributions to Your HSA › You will need to open an account with Fidelity (instructions below.) This will allow your payroll contributions and the UnityPoint Health contribution to be deposited at Fidelity. › In order to make pre-tax contributions to your HSA, you will need to elect those contributions within the Fidelity website. This will be the only method of making and changing your contributions throughout the year. Opening an account with Fidelity When you’re ready, opening and managing your HSA with Fidelity is fast and easy. You’ll get information on investment choices, payment options, and ongoing support to help you build and manage your savings. For convenience, you can open a Fidelity HSA online. Here’s how it works: › Log into NetBenefits® at NetBenefits.com › From the home page, click “Open” next to Health Savings Account. › If you do not have access to NetBenefits, contact a Fidelity Representative at 1-800-544-3716.
| 14 | HSA Account Transfer Process To transfer an HSA account from another provider, team members must first set up their Fidelity HSA: 1 Log in to NetBenefits.com. 2 Click the “Open” link next to “Health Savings Account.” Follow the online instructions. Establishing a Fidelity HSA is not automatic. › After the Fidelity HSA is open, team members may transfer savings from other HSA providers. › Fidelity can coordinate the transfer for team members and does not charge a fee for this transaction. › This transfer is not considered a taxable event and will not be reported to the IRS. › The assets being transferred are not applied toward the team member’s HSA maximum annual contributions limit. To transfer other HSA assets team members can click here. 2024 Annual HSA Contribution Limits* Individual health care coverage $4,150** Family health care coverage $8,300** Additional catch-up contribution (if age 55 or older) $1,000** * Please remember to not exceed the annual IRS HSA contribution limit, which is the total of your personal contribution plus UnityPoint Health contribution. ** The maximum amount you may contribute to your HSA, assuming you enroll at the start of 2024. These amounts include UnityPoint Health contributions. If you enroll into an HSA after the first of the year, this amount will change based on the monthly prorated UnityPoint Health contribution. Health Savings Account (HSA), continued
| 15 | Dental Insurance Which Dental Plan is the best choice for Me? We offer dental coverage through Delta Dental with a choice of two plans: BASIC and PREMIER. Both dental plans provide coverage for preventive and basic care services. BASIC PLAN: › Lower premiums › Doesn’t cover orthodontia or major services PREMIER PLAN: › Covers orthodontia in full if under 19 › Covers major services SAVE MONEY ON THE BASIC PLAN If you and your eligible dependents don’t have orthodontia (under age 19) or major dental service needs, the Basic Plan offers you a way to save money while still getting coverage for your diagnostic, preventive and routine restorative services. DELTA DENTAL PPO NETWORK When you see a dental provider who is in the Delta Dental PPO network, you will commonly pay less than when you see a dental provider who is in the Delta Dental Premier network or an out-of-network provider. The Enhanced Benefits Program (EBP) is available under both plans. The EBP offers additional oral health services to Eligible Covered Persons with qualifying dental or medical conditions. Qualifying participants may be eligible for additional cleanings and topical fluoride application. Coverage and Costs Delta Dental contracts with dentists and other dental care providers in all of the communities where UnityPoint Health affiliates are located. You can review the coverage levels and premium information for each dental plan on the next page to help you determine which plan is best for you. The percentages in the table are the percentages you pay.
| 16 | Dental Insurance, continued BASIC PLAN PREMIER PLAN Delta PPO*** Delta Premier/ Out of Network Delta PPO*** Delta Premier/ Out of Network Deductible $25 $50 $15 $25 Individual Annual Maximum* $750 $750 $1,500 $1,500 Diagnostic & Preventive Exams, cleanings, space maintainers, Sealants, X-rays, Fluoride (Dependent Children Under 19) 100% covered 100% covered Routine Restorative Services Simple extractions, surgical services 10% after deductible 20% after deductible 10% after deductible 20% after deductible Emergency Treatment Routine Oral Surgery Posterior Composites 50% after deductible 50% after deductible Major Services Endodontics – root canal therapy Not covered 20% after deductible Periodontics – conservative and maintenance therapies Periodontics – complex procedures 50% after deductible Crowns, inlays, onlays Bridges and dentures Repairs and adjustments Orthodontics (Dependent Children Under 19) Appliances, treatment & related services Not covered 50% after deductible Lifetime Maximum** per dependent child $2,000 Dental Premium Cost – Per Pay Period Employee Only $5.89 $9.54 Employee + Child(ren) $13.20 $21.63 Employee + Spouse/DP $11.58 $19.05 Family $17.50 $28.85 *The Individual Annual Maximum is the maximum benefit each covered person is eligible to receive for certain covered services in 2024. **The Lifetime Maximum is the maximum benefit each covered person is eligible to receive for orthodontics in a lifetime. *** You will commonly pay less when seeing a Participating Delta Dental Dentist. For more information, please see the Dental SPD located on the HR Landing Page.
| 17 | Vision Insurance Vision Examination IN-NETWORK OUT-OF-NETWORK Includes refraction Covered in full after $10 copay Up to $35 Retinal Imaging Up to $45 member out-of-pocket (OOP) maximum N/A Materials $10 copay (Materials copay applies to frame or spectacle lenses, if applicable.) Frame Allowance Up to 20% discount above frame allowance.* Members receive a $65 wholesale allowance up to $175 retail value† Up to $55 Standard Spectacle Lenses Single Vision Covered in full after $10 copay Up to $25 Bifocal Up to $40 Trifocal Up to $50 Lenticular Up to $80 Preferred Pricing Options Level 6 Option Package Polycarbonate (Single Vision/Multi-Focal) $40/$44 (Covered in full up to age 19) N/A (Up to $10 for ages up to 19) Standard Scratch-Resistant Coating $17 N/A Ultraviolet Screening $15 Solid or Gradient Tint $17 Standard Anti-Reflective Coating $45 Under the vision plan, you may purchase your eyeglasses and contacts at the eye care provider of your choice. When you use an Avesis network provider, you receive the highest level of plan benefits and have the lowest out-of-pocket costs. For routine eye exams, you can see any Optometry provider; in or out-of-network. However, for non- routine eye care, you’ll need to visit an in-network provider. † Value may be less depending on the providers retail pricing. * Discounts are not insured benefits. ‡ Enhanced benefit for certain conditons. ¥ Save up to 25% on average LASIK prices when you use Qualsight (visit qualsight.com/-avesis for more information).
| 18 | Vision Insurance, continued Preferred Pricing Options, continued Level 1 Progressives Covered in full Up to $40 Level 2 Progressives Covered in full Up to $48 All Other Progressives $140 allowance + up to 20% discount Up to $48 Transitions® (Single Vision/ Multi-Focal) $70/$80 n/a Polarized $75 PGX/PBX $40 Other Lens Options Up to 20% discount* Contact Lenses (In lieu of frame and spectacle lenses) Elective $175 allowance Up to $160 Medically Necessary** Covered in full Up to $250 Refractive Laser Surgery Up to 25% provider discount ¥ Onetime/lifetime $150 allowance Provider discount up to 25%* Onetime/lifetime $150 Frequency Eye Examination Once every 12 months Lenses or contact lenses Once every 12 months Glasses Frames Once every 24 months Vision Premium Cost Employee Only Employee + Child(ren) Employee + Spouse/DP Family Full & Part Time Rates $3.29 $7.16 $6.32 $9.38
| 19 | Flexible Spending Accounts (FSA) Flexible Spending Accounts (FSAs) give you the opportunity to lower your taxes by paying for eligible health care and dependent care expenses on a pretax basis. You choose whether to participate in one or both of the accounts during each year. The FSAs are funded entirely with your contributions, which are made with pretax dollars from your paycheck. Eligible Expense Reimbursement: 2024 FSA Plan Funds For your 2024 plan year, you will be able to submit an eligible expense with a date of service between January 1, 2024 and December 31, 2024 and be reimbursed with your 2024 plan year funds. All eligible claims must be submitted by March 31, 2025. As you choose to participate, there are a few things to keep in mind: UNDERSTAND THE “USE-IT- OR-LOSE-IT” RULE. Unspent money left in your FSA accounts is forfeited after the end of the year. EACH ACCOUNT IS SEPARATE. You cannot transfer money between the health care and dependent care accounts. NO AUTOMATIC RENEROLLMENT IRS rules require you to actively re- enroll in the FSAs each year if you want to contribute pretax dollars. SAVE YOUR RECEIPTS. You may be required to submit them to HealthPartners to document your expenditures. CHOOSE YOUR CONTRIBUTION AMOUNT WISELY. Once you choose your FSA contribution amount, your election cannot be changed during the year without a qualifying life event. ENROLL IN DIRECT DEPOSIT. The fastest way to get your reimbursement is to enroll in direct deposit. Besides accessing your reimbursement faster, you’ll also avoid a fee of $5 per reimbursement check issued.
| 20 | Health Care FSA › This account is for eligible health care expenses for you and your dependents. › Eligible expenses include medical, dental, orthodontia, vision and hearing aid expenses not covered by another health benefit plan. › You can contribute up to $3,050 to your Health Care FSA in 2024. Limited Use FSA › If you enroll in the Health Savings Plan, you cannot have a regular Health Care FSA, but you can have a Limited Use FSA. › With the Limited Use FSA, eligible expenses include dental, orthodontia and vision expenses — not medical or prescription drugs. › You can contribute up to $3,050 to your Limited Use FSA in 2024. Dependent Care FSA › This account can be used to pay dependent care expenses for children under 13 or adult dependents who can’t care for themselves. › Qualified expenses include in-home child care, licensed day care, preschool facilities, before- or after-school programs, and elder care. › You can contribute up to $5,000 to your Dependent Care FSA in 2024. Note: If your spouse also participates in a dependent care FSA, the tax-free benefit is limited to $5,000 for both of you combined. If you are married but filing taxes separately, the tax-free benefit is limited to $2,500. Flexible Spending Accounts (FSA), continued MANAGE YOUR FSA ON THE GO Download the free HealthPartners myHP app from the iTunes Store or Google Play to: › Check your account balances on the go. › Snap and submit photos of your receipts and file claims. › And more!
| 21 | Flexible Spending Accounts (FSA), continued Your FSA Debit Card When you enroll in the health care or limited use FSA, you will receive a debit card from HealthPartners, which you can use to pay for your eligible FSA expenses. Some card transactions will be verified at the point of purchase and others will be verified later through an automatic process. However, if HealthPartners cannot determine whether a transaction was for an eligible health care product or service, you will need to submit a detailed receipt to verify your purchase. You may also submit claims and requested documentation from the myHP mobile app. You can find more FSA resources at HealthPartners.com. If you have questions or need assistance with your FSA account, call HealthPartners Member Services at (888) 735-9200. How long do you have to use your debit card for plan year expenses? You shouldn’t use your debit card for expenses once the plan year has ended. For example, you shouldn’t use the card in 2025 for 2024 expenses. If you still have 2024 expenses to submit in 2025, you’ll need to do it in the app, online, by mail, or fax. FSA TIPS & RESOURCES Tips to help automatically approve your expenses: › Pay your bill in full as soon as possible. › Pay separately for each date of service. Tips for submitting documentation: › Save your documentation electronically so it’s easy to attach to your reimbursement request. You can take a picture with your smartphone or scan it. Submit your reimbursement request using the myHP mobile app or your myHealthPartners account. You can also mail or fax a copy to HealthPartners at (877) 624-2287. › Keep all receipts. › If you don’t have a HealthPartners medical plan, get a copy of your Explanation of Benefits (EOB). › Read all letters and emails from HealthPartners. They let you know when documentation is needed. › Send in documentation right away. Your card could be suspended if you wait too long. If documentation is requested and not received you may be taxed on the amount of the transaction. Additional FSA resources can be found at HealthPartners.com. If you have questions or need assistance with your FSA account, call HealthPartners Member Services at (888) 735-9200.
| 22 | Life and Accidental Death & Dismemberment Insurance Life insurance coverage helps protect your loved ones in the event of your death or serious injury. Even if you’re single, your beneficiary can use your life insurance benefits to pay off your debts, such as credit cards, mortgages and other final expenses. Accidental Death & Dismemberment (AD&D) insurance pays a benefit if the covered person dies as a result of an accident. It will also pay all or part of the coverage amount if the covered person suffers a dismemberment injury or other covered loss due to an accident. You can purchase coverage for yourself, your spouse/domestic partner, and/or your dependent children. Basic Life and AD&D Insurance UnityPoint Health offers group term life and AD&D insurance automatically at no cost to you. Voluntary Life and AD&D Insurance You may purchase additional life and AD&D insurance at favorable group rates. You pay for this coverage with after-tax dollars. Premiums for this coverage are shown in Lawson during your enrollment experience. COVERED PERSON COVERAGE AMOUNTS PREMIUM Full-time and part-time benefit eligible team members 1 times your base annual pay, up to $100,000 No cost to you COVERED PERSON COVERAGE AMOUNTS PREMIUM Employee Increments of $10,000 up to the lesser of: › 8 times your annual base pay, or › $500,000 Based on team member’s age as of January 1, 2024 Spouse/domestic partner Increments of $10,000 up to $100,000 Based on team member’s age as of January 1, 2024 Children (up to age 26) Flat amount of $5,000 or $10,000 per child Flat rate no matter how many children are covered REVIEW & UPDATE Review and update your beneficiaries with Prudential at prudential.com/mybenefits
| 23 | Amount Limit Due to Age If you are age 70 and over, the life and AD&D insurance benefit amount you are eligible for is reduced. Team members aged 70-74 will have life and AD&D insurance value at 65% of the benefit, and those aged 75 and over will have a life and AD&D insurance value of 50% of the benefit. What You Need to Know About Evidence of Insurability (EOI) When it comes to voluntary life and AD&D insurance, you may be required to provide Evidence of Insurability, or EOI, to the insurance carrier as part of the application process. › If you are newly benefit eligible and enrolling in life and AD&D insurance for the first time: – you may purchase voluntary employee life and AD&D coverage in increments of $10,000 up to the lesser of 8 times your annual base pay or $500,000, without providing EOI. – you may purchase voluntary spouse/ domestic partner life and AD&D coverage in increments of $10,000 up to $100,000, without providing EOI. › Each year after your initial enrollment period, you may increase your coverage for yourself and/or spouse/domestic partner by $10,000 (not to exceed the maximum) without providing EOI as long as you are currently enrolled in voluntary life and AD&D insurance. Life AD&D Insurance EOI Process › If you are currently enrolled in voluntary life and AD&D insurance and you elect an amount greater than $10,000 after your initial enrollment period, you will be required to submit EOI. If this is the case, you will receive an email with a link to an online questionnaire about you and/or your spouse/domestic partner’s health. You must complete the questionnaire in order for your requested coverage increase to be considered. › Based on the answers in your questionnaire, you may also need to get a basic physical exam. Life and Accidental Death & Dismemberment Insurance, continued DON’T BE DENIED Evidence of Insurability is important! Your coverage may be delayed or denied if you don’t submit EOI.
| 24 | Calculating Your Voluntary Life and AD&D Cost Follow these steps to calculate your bi-weekly voluntary Life and AD&D insurance premium: Enter the amount of Voluntary Life and AD&D Insurance you want: $ ________(1) Employee: Increments of $10,000, up to the lesser of 8x your base annual pay or $500,000 Spouse/Domestic Partner: Increments of $10,000 up to $100,000 Divide the amount in Line 1 by 1,000 and enter: $ ________(2) Use the chart above to find the bi-weekly cost for employee’s age and enter: $ ________(3) Multiply the amount in Line 2 by the amount in Line 3 and enter: This is your bi-weekly cost for Voluntary Life and AD&D Insurance $ ________(4) Note: Your cost can change if your coverage amount changes, your age changes, or if the insurance rates change. Bi-Weekly Voluntary Life and AD&D Insurance Premiums (per $1,000 of coverage) AGE EMPLOYEE AND SPOUSE/ DOMESTIC PARTNER* Under 25 $0.027 25-29 $0.031 30-34 $0.040 35-39 $0.044 40-44 $0.051 45-49 $0.074 50-54 $0.111 55-59 $0.203 60-64 $0.309 65-69 $0.563 70-74 $0.910 75+ $0.955 Children $0.026 Flat Rate *Premium based on team member’s age as of January 1, 2024 Life and Accidental Death & Dismemberment Insurance, continued
| 25 | Critical Illness Insurance COVERED PERSON COVERAGE AMOUNTS Employee $10,000 | $20,000 | $30,000 Spouse/domestic partner $10,000 Children $5,000 per child You must elect critical illness insurance for yourself in order to elect coverage for your spouse/domestic partner or child(ren). Watch the critical illness insurance video Critical Illness Insurance through Voya pays a lump sum benefit if you are diagnosed with a covered illness or condition. You can use the benefit payment for any purpose you choose. You can purchase coverage for yourself, your spouse/domestic partner, and your children under age 26. If you leave UnityPoint Health, you can take this coverage with you. The following coverage amounts are available: WELLNESS BENEFIT The plan also pays a wellness benefit of $50 once per calendar year for each family member enrolled when an eligible health screening test is completed. For more information, review the Wellness Benefit Claims Checklist & FAQ. If a covered person is diagnosed with a covered condition, the plan will pay this amount: 100% OF COVERAGE › Heart attack › Stroke › Coma › Cancer › Type 1 Diabetes › Major organ failure › Permanent paralysis › End stage renal failure 25% OF COVERAGE › Coronary artery bypass › Carcinoma in situ › Open heart surgery for valve replacement or repair 10% OF COVERAGE › Skin cancer › Transcatheter heart valve replacement or repair
| 26 | Critical Illness Insurance, continued Although there is not a pre-existing condition limitation on the Critical Illness plan, the plan will only cover illnesses/diseases that are diagnosed after the effective date of coverage. At the time of claim, each claimant will be asked to provide supporting medical documentation along with the Attending Physician’s Statement of Critical Illness/ Specified Disease form. *COVID-19 diagnosis must be confirmed by a medical professional. **A benefit is payable up to a maximum of 1 time per Covered Person per policy calendar year Infectious Condition Additional Benefit Rider If you are diagnosed with COVID-19*, this pays a benefit** of $100. If you are hospitalized for COVID-19* and there is a room and board charge for that hospitalization, this pays a benefit** amount of $1,000. Specified Conditions Diagnosis Benefit This benefit will pay you a Specified Condition Diagnosis benefit if you are diagnosed with autism spectrum disorder Level 3 on or after the coverage effective date. Specified Condition Facility Confinement Benefit If you are diagnosed with bipolar disorder or depressive disorder that results in a confinement to a hospital, rehabilitation facility or transitional care facility, this benefit will pay you a Specified Condition Facility Confinement Benefit.
| 27 | Critical Illness Insurance: Bi-Weekly Premiums PREMIUMS - EMPLOYEE (BI-WEEKLY) $10,000 $20,000 $30,000 Age 29 and under $2.22 $4.43 $6.65 Age 30-34 $2.77 $5.54 $8.31 Age 35-39 $2.77 $5.54 $8.31 Age 40-44 $5.22 $10.43 $15.65 Age 45-49 $5.22 $10.43 $15.65 Age 50-54 $10.15 $20.31 $30.46 Age 55-59 $10.15 $20.31 $30.46 Age 60-64 $14.68 $29.35 $44.03 Age 65-70 $18.88 $37.75 $56.63 Age 70+ $25.48 $50.95 $76.43 PREMIUMS - SPOUSE/DOMESTIC PARTNER (BI-WEEKLY) $10,000 Age 29 and under $2.68 Age 30-34 $3.18 Age 35-39 $3.18 Age 40-44 $6.00 Age 45-49 $6.00 Age 50-54 $12.55 Age 55-59 $12.55 Age 60-64 $19.15 Age 65-70 $21.92 Age 70+ $33.05 PREMIUMS - CHILD (BI-WEEKLY $5,000 Per Family Unit $1.41
| 28 | Accident Insurance Accident Insurance also pays benefits for accident- related transportation, lodging, family care, prosthetic devices, burns, eye injuries, lacerations, dislocations, fractures and more. ACCIDENT INSURANCE: BI-WEEKLY PREMIUMS Employee Only $4.69 Employee + Spouse/ Domestic Partner $7.70 Employee + Child(ren) $8.91 Family $11.92 Your coverage also includes accidental death and dismemberment benefits. If you are severely injured or pass away due to an accident additional benefits may apply. Watch the accident insurance video Accident Insurance through Voya pays you benefits for specific injuries and events resulting from a covered accident. You can purchase coverage for yourself, spouse/domestic partner, and your children under age 26. If you leave UnityPoint Health, you can take this coverage with you. The amount paid depends on the type of injury and care received. For those who experience an accident claim and visit a UnityPoint Health facility, you will receive an additional 25% benefit up to $1,000. You can use the payments for any purpose you choose. Here are some examples of payment provided: EVENT/CONDITION BENEFIT AMOUNT EVENT/CONDITION BENEFIT AMOUNT Ground ambulance $400 Coma (14 or more days) $18,500 Air ambulance $2,000 Surgery (open abdominal, thoracic) $1,500 Emergency room treatment $250 Follow-up doctor visit $100 Hospital admission $1,500 Medical equipment $275 Hospital confinement (per day, up to 365 days) $375 Physical or occupational therapy (per treatment, up to 6) $60 Critical care unit confinement (per day, up to 15 days) $600 Mental health therapy (up to 10 per accident) $60 WELLNESS BENEFIT The plan also pays a wellness benefit of $50 once per calendar year for each family member enrolled when an eligible health screening test is completed. For more information, review the Wellness Benefit Claims Checklist & FAQ.
| 29 | Hospital Indemnity Insurance Watch the hospital indemnity insurance video What is Hospital Indemnity Insurance? Hospital Indemnity Insurance through Voya pays a daily benefit if you have a covered stay in a hospital, critical care unit or rehabilitation facility. The benefit amount is determined by the type of facility and the number of days you stay. Hospital Indemnity Insurance is not health insurance and does not satisfy the requirement of minimum essential coverage under the Affordable Care Act. How can Hospital Indemnity Insurance help? Below are a few examples of how your Hospital Indemnity Insurance benefit could be used (coverage amounts may vary): MEDICAL EXPENSES, SUCH AS DEDUCTIBLES AND COPAYS TRAVEL, FOOD AND LODGING EXPENSES FOR FAMILY MEMBERS EVERYDAY EXPENSES LIKE UTILITIES AND GROCERIES CHILD CARE Who is eligible for Hospital Indemnity Insurance? › All UnityPoint Health benefit eligible team members, their spouses/domestic partners and children. › Your children are eligible for coverage up to age 26. › If you elect coverage for your family members, your spouse/domestic partner and children will have the same Hospital Indemnity benefits as you do.
| 30 | How much does Hospital Indemnity Insurance cover? STANDARD BENEFIT BENEFIT AT UPH FACILITY Hospital Admission $1,000 $1,250 Critical Care Unit Admission $2,000 $2,500 Hospital Confinement $100/day, up to 30 days $125/day, up to 30 days Hospital Intensive Care $200/day, up to 15 days $250/day, up to 15 days Rehabilitation Facility Benefit $50/day, up to 30 days $62.50/day, up to 30 days Pregnancy Covered? Yes Yes Pre-Existing Condition Exclusion? No Portable and Transferable? Yes Bi-Weekly Premium Rates Employee $9.39 Employee + Spouse/DP $18.20 Employee + Child(ren) $13.79 Family $22.60 Hospital Indemnity Insurance, continued
| 31 | Short-Term Disability & Long-Term Disability Short-Term Disability (STD) The Short-Term Disability (STD) Plan provides income protection if you become disabled and cannot work due to a non-work-related illness or accidental injury. UnityPoint Health automatically provides Short-Term Disability coverage – at no cost to you – for all eligible team members. Participation begins on the first of the month following your start date or benefit status change date. The Short-Term Disability Plan begins to pay benefits after 14 days of continuous disability. Short-Term Disability benefits replace 60% of your regular weekly base pay, to a maximum of $2,500 per week, for up to 26 weeks. NO COST TO YOU UnityPoint Health automatically provides Short- Term and Long-Term Disability coverage- at no cost to you- for all eligible team members. Long-Term Disability If you become disabled for an extended period of time and cannot work, no benefit becomes more important to your financial security than disability income protection. BASIC LONG-TERM DISABILITY If you remain totally disabled and unable to work for more than 180 days, you may be eligible for Long-Term Disability (LTD) benefits through Prudential. UnityPoint Health automatically provides you LTD benefits that replace up to 50% of your monthly base pay, up to a maximum of $10,000 per month. Monthly LTD benefits will be reduced by Social Security and any other disability income you are eligible to receive, such as Workers’ Compensation. BUY-UP LONG-TERM DISABILITY You can purchase additional LTD coverage through Prudential that will increase your monthly benefit to 60% of your monthly pay. The cost of this additional coverage is available in Lawson during your enrollment. ABSENCEONE All approved Leaves of Absence (LOA), including intermittent FMLA and continuous LOA, including Short-Term Disability (STD), medical, personal, and military leave, are administered through AbsenceOne. Access the AbsenceOne online portal at AbsenceOne.com/ unitypointhealth.
| 32 | Legal Insurance & Identity Theft Protection Whether you need assistance writing your will, disputing a traffic ticket, or protecting yourself against identity theft, Legal Insurance and Identity Theft protection from ARAG is here to help. For only $9.46 per pay period, you and your covered dependents will have access to a nationwide network of attorneys who will work with you to address and resolve life’s legal, financial, and identity theft issues, such as: › Consumer and fraud protection › Wills and estate planning › Real estate › Family law › Civil damage claims (defense) › Criminal matters › Government benefits › Small claims court › Tax issues › Traffic matters › Debt-related matters › Landlord disputes In the event that your identity is stolen, the ARAG Identity Theft Protection program provides full-service restoration including access to Certified Identity Theft Restoration Specialists and reimbursement for up to $1 million for expenses associated with restoring your identity. To see a full list of coverages available under this plan, visit ARAGLegalCenter.com (access code 18191uph) and click on Plan Details. For any legal matters not covered and not excluded under the plan (including immigration assistance), you are eligible to receive at least 25% off the Network Attorney’s normal rate. Diversity, Equity & Inclusion Coverage ARAG is constantly evolving and adapting to meet the needs of all team members. Whether it’s a team member with a disability, a veteran or a member of the LGBTQ+ community, their coverage provides solutions that include: › Domestic Partnership Agreement › HIPAA/Hospital Visitation Authorization › Funeral Directive › Gender Identifier Change › Social Security/Veterans/ Medicare Dispute › School Administration Hearing and, network attorney fees for most covered matters like these are paid 100% in full. TRACK YOUR ACTIVITY This service can track your credit activity or online identity and you are notified immediately of suspicious activity.
| 33 | Watch the pet insurance video Pet Insurance Now more than ever, pets are playing a significant role in our lives, and it’s important to keep them safe and healthy. Help make sure your furry family members are protected against unplanned vet expenses for covered accidents or illnesses with MetLife Pet Insurance. Like health insurance for you and your family, pet insurance is coverage for dogs and cats that can help you be prepared for unexpected vet costs. With MetLife Pet Insurance, you may be able to cover up to 100% of the veterinary care expenses from any licensed veterinarian, specialist, or emergency clinic across the U.S. What are the coverage options? Coverage is flexible and customizable so that you can choose the plan that works for you. Options include: › Levels of coverage from $500 – unlimited › $0 - $2,500 deductible options › Reimbursement percentages from 50% - 100% How much does Pet Insurance cost? Each pet’s premium will be unique based on the age, breed, location, as well as what coverage amount you select. Plus, if you go claim-free in a policy year, MetLife will automatically decrease your deductible by at least $25. How do you pay for the insurance? You can set up an automatic payment from your bank or credit card with MetLife. WHAT’S COVERED? COVERAGE ALSO INCLUDES Exam fees Hip dysplasia Accidental injuries Hereditary conditions X-rays and diagnostic tests Congenital conditions Surgeries Chronic conditions Medications Alternative therapies Ultrasounds Holistic care Illnesses And much more! Hospital stays GET A QUOTE OR ENROLL To get a quote or enroll, visit metlife.com/getpetquote or call (800) GET-MET8.
| 34 | We are proud to invest in your financial health and future by continuing to provide a core contribution to you that is equal to 2% of your pay and also matching 50% for each dollar you contribute to your 401(k), up to the first 6%. To maximize your employer match, you would want to contribute 6% of your paycheck so you can receive the full 3% match from UnityPoint Health. While there isn’t any action required on your behalf for your enrollment, we do encourage you to log into the Fidelity portal (netbenefits.com). From there you can do things like: CHANGE YOUR INVESTMENTS UPDATE YOUR BENEFICIARIES DETERMINE HOW MUCH YOU SHOULD BE SAVING CHANGE YOUR CONTRIBUTIONS GET HELP WITH YOUR FINANCES BY TALKING TO A RETIREMENT PLANNER GET A SNAPSHOT OF YOUR RETIREMENT BY ANSWERING A FEW QUESTIONS Check out the Financial Wellness Portal for an interactive experience that brings together resources and tools you need to plan your financial wellness strategy. Retirement Savings and Financial Wellness SPEAK WITH A FIDELITY REPRESENTATIVE To speak with a Fidelity representative who can answer your questions or to schedule a one-on-one consultation, you can call (800) 343-0860. ELIGIBILITY You are eligible to participate in the retirement savings plan once you have reached age 19.
My Well-Being Programs, activities and resources designed to enhance physical, financial and emotional well-being
| 36 | Paid Time Off (PTO) The chart below will help provide you with details on our system-wide PTO plan. The purpose of PTO is to give team members flexibility in scheduling time away from work. PTO combines vacation, individual or family related sick days, holidays, and personal days you might need during the year. The PTO plan includes time off required under all state and local paid leave laws to include sick and safe leave. UnityPoint Recognized Holidays: New Year’s Day, Memorial Day, Fourth of July, Labor Day, Thanksgiving Day, Christmas Day. UnityPoint Health PTO Accrual Chart YEARS OF SERVICE COMPLETED PTO ACCRUED PER HOUR* MAXIMUM ANNUAL ACCRUAL* (BASED ON 2080 HOURS ANNUALLY) MAXIMUM CARRYOVER 0-1 0.09231 192 hours / 24 days 320 2-3 0.10385 216 hours / 27 days 320 4-8 0.11539 240 hours / 30 days 320 9-13 0.13847 288 hours / 36 days 320 14+ 0.16154 336 hours / 42 days 320 * To calculate your PTO accrual per pay period, multiply the “PTO Accrued per Hour” number above by the number of hours you are paid per pay period (not to exceed 80 hours per pay period or 2080 hours annually). For example, if you are a team member who has 16 years of service and are a .75 FTE or work 60 hours per pay period, your calculation to project your PTO accrual in the future would be as follows: 0.1615 x 60 = 9.69 accrued hours in a pay period. * In order to receive a PTO Cash election, you must be an active, benefit eligible team member at the time of the payout. Executives and Physicians are not eligible for PTO Cash. ** PTO cash elections can only be made within the election period. You will not be able to make changes, including cancellation, to your PTO cash election(s) outside of the election period. *** While there is no required remaining balance, if you elect to cash out more hours than you have in your bank at the time of the payout dates, you will not receive the full elected cash-out amount. Instead, your payout will be reduced to the number hours in your bank at the time of the payout. PTO Cash Benefit eligible team members are eligible to cash out up to 40 hours of PTO, in 5-hour increments, annually. Please review the information below for further details and contact AskHR if you have questions. › Component PTO Cash Guidelines › Maximum Hours to Declare 40 hours › Election Period** During Open Enrollment › Payout Dates Announced during the annual open enrollment period › Eligibility* Active, benefit eligible team members who are budgeted to work 32 hours or more per pay period (0.4 FTE or more). Executives and Physicians are not eligible for PTO Cash. › Required Remaining Balance*** There is no requirement to have any remaining balance in your PTO account after the cash out occurs.
| 37 | Parental Leave & Adoption Assistance Parental Leave We know it is important for you to take time to care for your newborn or adopted child. Any full-time benefit eligible team member (0.8 FTE or more) who has at least six months of employment with UnityPoint Health will have the ability to: › Receive 40 hours of additional Paid Time Off (PTO) › Utilize a position- guaranteed leave ABOUT YOUR BENEFIT When you request a parental leave following the birth or adoption of a child, UnityPoint Health will provide 40 hours of additional Paid Time Off (PTO). The additional days will be added to your PTO bank and can be used through your regular time off request. UnityPoint Health will also extend a position-guaranteed leave for two additional weeks. This extension will take place upon the exhaustion of Family Medical Leave Act (FMLA), Wisconsin Family and Medical Leave Law (WFMLL), Iowa Pregnancy Leave Law (IPLL), and/or Short- Term Disability. These additional two weeks must be taken consecutively. ABSENCEONE To speak with an AbsenceOne representative who can answer your questions or to request a Parental Leave, please contact AbsenceOne by visiting absenceone. com/unitypointhealth or calling (877) 467- 2671. Adoption Assistance UnityPoint Health will grant up to $6,000 in reimbursement, per child, for expenses related to the process of the legal adoption of a child to full-time and part-time benefit eligible team members who have completed at least 90 days of employment. For reimbursement, benefit eligible team members must complete the Application for Assistance and provide a copy of finalized adoption paperwork along with copies of appropriate bills, invoices, receipts, or other statements that verify the amount of adoption assistance being requested. This is done by submitting a case in Lawson to AskHR. If both parents work for UnityPoint Health, the total amount of reimbursement per legal adoption of a child is up to $6,000 per child.
| 38 | Team Member Discounts Team Member Discounts UnityPoint Health partners with PerkSpot to provide a one-stop shop for thousands of exclusive discounts in more than 25 categories including: › Restaurants › Clothing and Jewelry › Gym Memberships › Vehicles and Car Services › Electronics and Cell Phones › Home Services › Insurance › Office Supplies › Movie and Entertainment Tickets › Sports › Hotels › Flights PerkSpot is a free benefit to all UnityPoint Health team members. Visit https://unitypoint.perkspot.com to get started. DID YOU KNOW? If you would like to suggest a merchant for PerkSpot to work with, you can log in and click the “Suggest a Merchant” link in the upper right corner of the screen. Once you submit the suggestion, PerkSpot will contact the merchant. Merchants can also contact PerkSpot directly by calling 866-606-6057 if they would like to offer a discount to you and others. Earned Wage Access UnityPoint Health partners with Wisely by ADP to offer flexible pay options for our team members. You can request your earned wages through either the myWisely app (if you currently receive your paychecks through Wisely) or the DailyPay app. The available balance is based on your regular compensation and hours (minus any withholdings) worked to date during a pay period. Learn more here.
| 39 | OnPoint for Health: Wellness Credit and Wellness Rewards 2025 Wellness Credit Team members and their spouses or domestic partners who are enrolled in the health plan will have two opportunities to earn rewards – A wellness credit and a wellness reward. Please note: New hires as of October 1, 2024 and on will be grandfathered into the 2025 Wellness Credit. 1 Complete an annual physical with your primary care provider (PCP) between December 1, 2023 - November 30, 2024. 2 Log into the OnPoint for Health portal between October 1, 2024 - December 20, 2024 to complete the online Health Risk Assessment (HRA). 2024 Wellness Rewards Benefit-eligible team members (even if they are not enrolled in a UnityPoint Health medical plan) and their spouse/domestic partner (who must be enrolled in a UnityPoint Health medical plan) can earn points by completing challenges that will be available after January 1, 2024 in order to earn financial rewards. ACHIEVE 1,500 POINTS earn a $100 REWARD paid out on your paycheck ACHIEVE 3,000 points earn a $150 REWARD paid out on your paycheck Please note: All wellness rewards are subject to tax and you must be in an active, benefit-eligible status at the time the reward is paid out in order to receive it. * Eligibility for these rewards will be reviewed on a monthly basis between February and December 2024. The financial reward will be paid out by the 2nd paycheck of the following month in which the point total is achieved. DID YOU KNOW? Both UnityPoint Health medical plans completely cover the cost of your annual physical with your PCP. HEALTH RISK ASSESSMENT (HRA Review the Notice Regarding Wellness Program for information on what will be collected, how it will be used, who will receive it and what will be done to keep it confidential.
My Growth & Development Learning, career opportunities and other experiences that support professional and personal growth
| 41 | Education Assistance Benefits UnityPoint Health offers tuition assistance to eligible Team Members who seek to pursue education that supports the current business needs and future objectives of the organization. All education programs must be related to Team Member’s current job or an established career path within UnityPoint Health. Visit the HR Landing page for more information. Tuition Reimbursement FULL-TIME and PART-TIME BENEFIT ELIGIBLE TEAM MEMBERS who have been actively employed with UnityPoint Health for at least six months are eligible for Tuition Reimbursement. Team members must be in good standing and have not had a formal performance corrective action plan within the previous 12 months. Reimbursement Amounts CLASSIFICATION MAXIMUM AMOUNTS Full Time (64-80) $5,250/year Part Time (32-63) $2,625/year Terms of Tuition Reimbursement › All courses related to a degree or certificate program must be completed with a minimum grade equivalent of C or better and award college credit. Courses that are based on a pass/fail grading system must be completed with a passing grade. Courses in which a Team Member receives an incomplete, withdrawal, or equivalent grade are ineligible. › Eligible expenses include tuition, required textbooks, and mandatory course-related fees such as registration or admissions fees, lab fees, technology fees, library cards, and graduation fees. › Ineligible expenses include, but are not limited to, meals, lodging, transportation and tools or supplies (other than textbooks) that can be kept after completing the course of instruction › Educational programs not covered include, but are not limited to, individual courses for sports, recreation or hobbies, unless part of a degree program and seminars, conferences and workshops. › Although attainment of educational goals often leads to improved performance and new career opportunities, participation in this program does not guarantee a specific career result such as a promotion or salary increase. › In compliance with IRS regulations (section 127), employer provided educational assistance is exempt from taxation up to a maximum of $5,250 per calendar year. Taxes will be assessed if, at the time of payment processing, the total amount of tuition assistance paid in the calendar year exceeds $5,250. Please consult with your tax advisor for additional information.
| 42 | Education Assistance, continued Work Commitment A Team Member who voluntarily terminates employment or is terminated for cause within 12 months of receiving education assistance through Traditional Reimbursement will be required to refund UnityPoint Health 100% of the payments received within that time period on a pro-rated basis from the time of last payment and date of termination. Public Service Loan Forgiveness (PSLF) Support PSLF is a federal program created for those in public service jobs, offering the opportunity to have your federal loan balances forgiven after 10 years and 120 qualifying payments. All tax free! Team Members can receive PSLF support through Fidelity’s Summer program aimed at streamlining and automating the process while reducing stress with resources that may help increase financial well- being and confidence. KEY FEATURES OF THE PROGRAM INCLUDE: › Complete PSLF coverage – Summer manages the entire PSLF process for borrowers from checking eligibility to employer coordination and online form submission. › Recertification support – Summer works with borrowers and their employers to ensure all PSLF requirements are met. › Protection from server mistakes – Summer has deep experience navigating rejections from loan servicer mistakes. For help from an expert to determine your eligibility or support filling in your forms, visit fidelity.com/forgiveness. Employment certification forms ready for completion should be sent to [email protected]. Student Loan Origination & Refinancing Fidelity’s Credible program is one way to find options to pay for college. Credible is an online marketplace that provides borrowers looking for private student loads with competitive, personalized, prequalified rates from up to 8 vetted lenders. There is no cost to request offers, and checking rates will not impact your credit score. Key features of the program include: › Personalized rates, not ranges from multiple lenders › Ability to comparison shop across lenders to find the best solution for your situation › No hidden fees, original fees, or prepayment penalties › Simple online process that keeps your data confidential. To access Credible log into the Fidelity portal at netbenefits.com.
| 43 | This booklet highlights the main features of the benefit plans sponsored by UnityPoint Health. Full details of these benefits are contained in the legal documents governing the plans. If there is any discrepancy or conflict between the plan documents and the information presented here, the plan documents will govern. In all cases, the plan documents are the exclusive source for determining rights and benefits under the plans. UnityPoint Health reserves the right to change or discontinue the plans at any time with appropriate notification. Participation in the plans does not constitute an employment contract. UnityPoint Health reserves the right to modify, amend, or terminate any benefit plan or practice described in this booklet. Nothing in this booklet guarantees that any new plan provisions will continue in effect for any period. Plan documents are available at the HR landing page on the Hub or by contacting AskHR at (888) 543-2275.
Appendix
| 45 | UNITYPOINT HEALTH PAYS FOR › Health Savings Account (Employer Contribution) › Basic Life and AD&D Insurance › Short-Term Disability › Long-Term Disability › Employee Assistance Program (EAP) › Paid Leave (Bereavement, Jury Duty, Parental Leave, etc.) › OnPoint for Health Wellness Program › Education Assistance › Paid Time Off (PTO) › 401(k) Employer Match YOU PAY FOR › Health Savings Account (Employee Contributions) › Vision Insurance › Voluntary Life and AD&D Insurance › Legal Insurance & Identity Theft Protection › Flexible Spending Accounts (FSA) › Critical Illness Insurance › Hospital Indemnity Insurance › Accident Insurance › Pet Insurance › 401(k) Employee Contributions Cost Breakdown You and UnityPoint Health (UPH) share the cost of your benefits. You pay your share of most benefit costs before federal, state and Social Security taxes are calculated. YOU AND UNITYPOINT HEALTH SHARE THE COST OF › Health Insurance* › Dental Insurance *UnityPoint Health pays for the majority of these costs Health Insurance EMPLOYEE ONLY EMPLOYEE + CHILD(REN) EMPLOYEE + SPOUSE/DP FAMILY Network Plan Full-Time Rates $79.82 $154.71 $188.09 $257.94 Part-Time Rates $119.73 $232.07 $282.13 $386.91 Health Savings Plan Full-Time Rates $47.05 $92.55 $112.50 $154.27 Part-Time Rates $71.63 $138.81 $168.75 $231.41 Premium amounts shown above do not include the working spouse surcharge. For more information, please refer to the Enrollment and Eligibility section. Dental Insurance Basic Plan – Full & Part Time Rates $5.89 $13.20 $11.58 $17.50 Premier Plan – Full & Part Time Rates $9.54 $21.63 $19.05 $28.85 Vision Insurance Full & Part Time Rates $3.29 $7.16 $6.32 $9.38 LISTED BELOW All premiums listed below are deducted over 26 pay periods
| 46 | Voluntary Life and AD&D Insurance (Bi-Weekly Premiums, per $1,000 of coverage) AGE EMPLOYEE & SPOUSE/ DOMESTIC PARTNER* AGE EMPLOYEE & SPOUSE/ DOMESTIC PARTNER* Under 25 $0.027 55-59 $0.203 25-29 $0.031 60-64 $0.309 30-34 $0.040 65-69 $0.563 35-39 $0.044 70-74 $0.910 40-44 $0.051 75+ $0.955 45-49 $0.074 Children $0.026 Flat Rate 50-54 $0.111 *Premium based on team member’s age as of January 1, 2024 Hospital Indemnity Insurance EMPLOYEE ONLY EMPLOYEE + CHILD(REN) EMPLOYEE & SPOUSE/ DOMESTIC PARTNER FAMILY $9.39 $13.79 $18.20 $22.60 Accident Insurance EMPLOYEE ONLY EMPLOYEE + CHILD(REN) EMPLOYEE & SPOUSE/ DOMESTIC PARTNER FAMILY $4.69 $8.91 $7.70 $11.92 Legal Insurance & Identity Theft Protection $9.46 for employee and all dependents Critical Illness Insurance PREMIUMS - EMPLOYEE (BI-WEEKLY) PREMIUMS - SPOUSE/ DP (BI-WEEKLY) PREMIUMS - CHILD (BI-WEEKLY) $10,000 $20,000 $30,000 $10,000 $5,000 Age 29 and under $2.22 $4.43 $6.65 $2.68 Per Family Unit $1.41 Age 30-34 $2.77 $5.54 $8.31 $3.18 Age 35-39 $2.77 $5.54 $8.31 $3.18 Age 40-44 $5.22 $10.43 $15.65 $6.00 Age 45-49 $5.22 $10.43 $15.65 $6.00 Age 50-54 $10.15 $20.31 $30.46 $12.55 Age 55-59 $10.15 $20.31 $30.46 $12.55 Age 60-64 $14.68 $29.35 $44.03 $19.15 Age 65-70 $18.88 $37.75 $56.63 $21.92 Age 70+ $25.48 $50.95 $76.43 $33.05
| 47 | Vendor Contact List PLAN CONTACT PHONE WEBSITE Health Insurance/ FSA HealthPartners (888) 735-9200 healthpartnersunitypointhealth.com/uph Dental Insurance Delta Dental of Iowa (800) 544-0718 deltadentalia.com Vision Insurance Avesis (855) 214-6777 avesis.com OnPoint for Health Applied Health Analytics (855) 581-9910 onpointforhealthuph.personal healthportal. net/login Health Savings Account (HSA) Fidelity (800) 544-3716 netbenefits.com Accident Insurance Voya Financial (877) 236-7564 voya.com Critical Illness Insurance Voya Financial (877) 236-7564 voya.com Life/AD&D/ Disability Prudential Life Inquires: (800) 524-0542 EOI Inquires: (888) 257-0412 www.prudential.com/mybenefits Hospital Indemnity Insurance Voya Financial (877) 236-7564 voya.com Legal Insurance & Identity Theft Protection ARAG (800) 247-4184 (access code 18191uph) ARAGLegalCenter.com Pet Insurance MetLife (800) GET-MET8 metlife.com/getpetquote Retirement Savings Fidelity (800) 343-0860 netbenefits.com Education Assistance EdAssist live chat available on website unitypoint.edassist.com UnityPoint Health IT Service Center UnityPoint Health (800) 681-2060 N/A
| 48 | ERISA Disclosure Notice UnityPoint Health does not discriminate, exclude, or treat people differently on the basis of race, color, national origin, age, disability, or sex. We provide the following for free: › Communication aids and services to people with disabilities, such as: – Sign language interpreters – Written information in other formats › Language services to people whose primary language is not English, such as: – Interpreters – Information written in other languages If you need these services, contact the Section 1557 Coordinator. If you believe that we have failed to provide these services or discriminated on the basis of race, color, national origin, age, disability, or sex, you can file a grievance in person, by mail or by phone with: Benefits Manager, Human Resources 1776 West Lakes Parkway West Des Moines, IA 50266 (515) 883-9662 The Section 1557 Coordinator is available to help you file a grievance. You can also file a complaint with the U.S. Department of Health and Human Services, Office for Civil Rights, electronically at https://ocrportal.hhs.gov/ocr/portal/ lobby.jsf, or by mail or phone at: U.S. Department of Health and Human Services 200 Independence Avenue, SW Room 509F HHH Building Washington, D.C. 20201 1-800-368-1019 | 1-800-537-7697 (TDD) Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html Vietnamese CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 1-515-574-6608. Arabic ﻣﻠﺣوظﺔ: إذا ﻛﻧت ﺗﺗﺣدث اذﻛر اﻟﻠﻐﺔ، ﻓﺈن ﺧدﻣﺎت اﻟﻣﺳﺎﻋدة اﻟﻠﻐوﯾﺔ ﺗﺗواﻓر ﻟك ﺑﺎﻟﻣﺟﺎن. اﺗﺻل ﺑرﻗم 1-515-574-6608 Chinese注意:如果您使用繁體中文,您可以免費獲得語 言援助服務。請致電 1-515-574-6608。 French ATTENTION : Si vous parlez français, des services d’aide linguistique vous sont proposés gratuitement. Appelez le 1-515-574-6608. German ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung. Rufnummer: 1-515-574-6608. Gujarati !ુચના: જો તમે -ુજરાતી બોલતા હો, તો િન:5ુ6ક ભાષા સહાય સેવાઓ તમારા માટ? ઉપલBધ છે. ફોન કરો 1-515-574-6608. Hindi !यान द': य)द आप ,हंदी बोलते ह5 तो आपके िलए मु;त म' भाषा सहायता सेवाएं उपलAध ह5। 1-515-574-6608 पर कॉल कर'। Hmong LUS CEEV: Yog tias koj hais lus Hmoob, cov kev pab txog lus, muaj kev pab dawb rau koj. Hu rau 1-515-574-6608. Italian ATTENZIONE: In caso la lingua parlata sia l’italiano, sono disponibili servizi di assistenza linguistica gratuiti. Chiamare il numero 1-515-574-6608. Korean주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다. 1-515-574-6608 번으로 전화해 주십시오. Polish UWAGA: Jeżeli mówisz po polsku, możesz skorzystać z bezpłatnej pomocy językowej. Zadzwoń pod numer 1-515-574-6608. Russian ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните 1-515-574-6608. Spanish ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-515-574-6608. Tagalog PAUNAWA: Kung nagsasalita ka ng Tagalog, maaari kang gumamit ng mga serbisyo ng tulong sa wika nang walang bayad. Tumawag sa 1-515-574-6608. Urdu .اﮔر آپ اردو ﺑوﻟﺗﮯ ﮨﯾں، ﺗو آپ ﮐو زﺑﺎن ﮐﯽ ﻣدد ﮐﯽ ﺧدﻣﺎت ﺑردار: ﻣﻔت ﻣﯾں دﺳﺗﯾﺎب ﮨﯾں ۔ ﮐﺎل ﮐرﯾں1-515-574-6608 . Availability of Summary Health Information UnityPoint Health offers two medical plans. As required by Patient Protection and Affordable Care Act, your plan makes available a Summary of Benefits and Coverage (SBC) for each option. The SBCs can be found at the HR landing page on the Hub. You can also request a paper copy, free of charge, by contacting AskHR
| 49 | HIPAA Notice of Special Enrollment Rights If you are declining enrollment for yourself or your dependents (including your spouse) because of other health insurance or group health plan coverage, you may be able to enroll yourself and your dependents in this plan if you or your dependents lose eligibility for that other coverage (or if the employer stops contributing toward your or your dependents’ other coverage). However, you must request enrollment within 30 days after your or your dependents’ other coverage ends (or after the employer stops contributing toward the other coverage). In addition, if you have a new dependent as a result of marriage, birth, adoption, or placement for adoption, you may be able to enroll yourself and your dependents. However, you must request enrollment within 30 days after marriage. You must request enrollment within 60 days of birth, adoption, placement for adoption, loss of eligibility for Medicaid or Children’s Health Insurance Program (CHIP) or becomes eligible for subsidy (state premium assistance program). To request special enrollment or obtain more information, contact UnityPoint Health’s AskHR department by calling 1-888- 543-2275. Women’s Health And Cancer Rights Act of 1998 (WHCRA) Do you know that your plan, as required by the Women’s Health and Cancer Rights Act of 1998, provides benefits for mastectomy-related services including all stages of reconstruction and surgery to achieve symmetry between the breasts, prostheses, and complications resulting from a mastectomy, including lymphedema? Call HealthPartners Member Services at (888) 735-9200 for more information. No Surprise Act Notice Federal law requires health insurance issuers offering group health insurance coverage to make available a notice to team members informing them of federal restrictions on balance billing and the requirements under Code 9816, ERISA section 716, and PHS Act second 2799A-1. The No Surprise Act Notice also lets you know how you may contact appropriate state or federal agencies if a provider or facility has violated the restrictions against balance billing. Premium Assistance Under Medicaid and The Children’s Health Insurance Program (CHIP) If you or your children are eligible for Medicaid or CHIP and you’re eligible for health coverage from your employer, your state may have a premium assistance program that can help pay for coverage, using funds from their Medicaid or CHIP programs. If you or your children aren’t eligible for Medicaid or CHIP, you won’t be eligible for these premium assistance programs, but you may be able to buy individual insurance coverage through the Health Insurance Marketplace. For more information, visit www.healthcare.gov. If you or your dependents are already enrolled in Medicaid or CHIP and you live in a state listed in the CHIP notice, contact your State Medicaid or CHIP office to find out if premium assistance is available. If you or your dependents are NOT currently enrolled in Medicaid or CHIP, and you think you or any of your dependents might be eligible for either of these programs, contact your State Medicaid or CHIP office or dial 1(877) KIDS NOW or www.insurekidsnow.gov to find out how to apply. If you qualify, ask your state if it has a program that might help you pay the premiums for an employer-sponsored plan. If you or your dependents are eligible for premium assistance under Medicaid or CHIP, as well as eligible under your employer plan, your employer must allow you to enroll in your employer plan if you aren’t already enrolled. This is called a “special enrollment” opportunity, and you must request coverage within 60 days of being determined eligible for premium assistance. If you have questions about enrolling in your employer plan, contact the Department of Labor at www.askebsa.dol.gov or call 1(866) 444-EBSA(3272). If you live in one of the states listed in the CHIP notice, you may be eligible for assistance paying your employer health plan premiums. Contact your state using the contact information provided here for more information on eligibility.
| 50 | Marketplace Notice The Patient Protection and Affordable Care Act (ACA) requires employers to provide team members with a written notice informing them of the existence of the Marketplace, including a description of the services provided by the Marketplace. The Marketplace Notice also lets you know how you may contact the Marketplace to request assistance. Illinois Consumer Coverage Disclosure For team members residing in Illinois, the Consumer Coverage Disclosure Act (CCDA) requires employers to disclose a written list of benefits offered compared to the list of essential health benefits issued by the State of Illinois. The Illinois Consumer Coverage Disclosure lets you compare the benefits offered by UnityPoint Health with the state’s ‘Benchmark Plan’ posted on the Illinois Department of Labor website. Notice of Privacy Practices The HIPAA Privacy Rule requires groups offering certain health benefit plans to develop and distribute a Notice of Privacy Practices (NPPs). The Notice of Privacy Practices must describe how the covered entity may and may not use protected health information (PHI) and what your rights and obligations with respect to protected health information (PHI) are. Voluntary Benefit Notice UnityPoint Health does not sponsor, endorse or administer these voluntary programs or benefits and these voluntary programs or benefits do not constitute an “employee benefit plan” under the Employee Retirement Income Security Act of 1974 (ERISA), as amended. › Accident Insurance › Critical Illness Insurance › Hospital Indemnity Insurance › Legal Insurance & Identity Theft Protection